Feeling overwhelmed? Learn how to deal with difficult elderly parents using practical, compassionate strategies for communication, boundaries, and care.
Navigating conversations with aging parents can feel challenging. The key often lies in gently shifting your own perspective. Before reacting to a frustrating behavior, it can be helpful to take a quiet moment and consider the why behind it. Often, what we see on the surface is a sign of something deeper—perhaps fear, frustration, or a sense of loss.

It can be unsettling when conversations with a parent, once a source of comfort, now feel unpredictable. Simple offers of help might be met with a sharp "I can do it myself," and genuine concern can be dismissed. If this sounds familiar, please know you are not alone.
This shift in family dynamics is happening in many homes. By 2030, it's estimated that one in six people worldwide will be aged 60 or older. This means millions of adult children are finding themselves in this new role, learning how to support parents who want to remain independent. The good news is that this desire is being met, with home care services now leading the elderly care market. You can explore more about these trends in elderly care and see just how many families are walking a similar path.
A helpful first step is to pause and look beneath the surface of a difficult behavior. These reactions are often not about us. They can be the outward expression of a tangled and sometimes painful internal struggle.
That stubborn refusal to accept help? It might be a way of holding on to the independence they've cherished their entire adult life. That irritable, dismissive tone could be masking the frustration of a body that no longer cooperates or a mind that feels a little less sharp.
When we reframe these behaviors, it can change our approach. This table can help connect what you're seeing to what they might be feeling.
| Observed Behavior | How It Might Feel to You | A Potential Underlying Reason |
|---|---|---|
| Refusing help with tasks they clearly struggle with | Frustrating, like they don't appreciate your effort | A deep-seated fear of losing their independence |
| Becoming easily irritated or angry over small things | Hurtful, as if you're the target of their anger | Chronic pain or physical limitations that create discomfort |
| Accusing you of nagging or being controlling | Confusing, when you're just trying to ensure their safety | Cognitive changes that may make them feel scared and defensive |
| Repeatedly telling the same stories | Tiring, making conversation difficult | Loneliness or a need to connect with cherished memories |
| Resisting changes to their home or routine | Stubbornness, an unwillingness to be flexible | A feeling that their world is shrinking and a desire to hold onto the familiar |
Seeing their actions through a lens of compassion doesn't excuse hurtful behavior, but it can help you take it less personally, allowing you to respond with more patience and grace.
By reframing their resistance as a sign of their desire for autonomy, you can approach conversations with more empathy and less frustration. It changes the goal from winning an argument to understanding their perspective.
Timing can make a big difference. Trying to discuss a sensitive topic when your mom is tired from an appointment or when you're rushing to get dinner ready is often a recipe for conflict.
Instead, look for a calm, low-pressure moment. This might be on a quiet drive, over a cup of coffee at the kitchen table, or while folding laundry side-by-side. The setting should feel neutral and safe, not like an ambush or an intervention.
When you bring something up, framing it as a simple observation from a place of love can be more effective than a judgment. "I noticed..." is often a better start than "You need to..." Your goal isn't to solve everything in one conversation. It's just to open the door a little. These small beginnings can build the trust you'll need for bigger conversations later on.
When a parent is described as "difficult," families often focus on the behavior itself—arguments, refusals, guilt trips, or emotional outbursts. What's easier to miss is how much of this tension comes from unspoken fear, role changes, and uncertainty about what's coming next.
Here are a few patterns families frequently overlook when interactions start feeling consistently hard:
Understanding these underlying dynamics doesn't excuse hurtful behavior—but it can help you respond with steadiness instead of escalating tension, especially when conversations need to move forward.
When these dynamics are at play, timing and approach matter even more than the words you choose. Difficult conversations rarely succeed when they feel rushed or reactive. Finding a calmer entry point can help reduce defensiveness and create space for more honest, productive dialogue.

It can be exhausting when every conversation feels like a potential disagreement. You might start avoiding important topics just to keep the peace. When you get to that point, it can be a sign that the old ways of talking aren't working anymore.
The goal isn't to win an argument. It's to open a door. The aim is to create a space where your parent feels heard and respected, not managed or controlled. This takes practical skills you can lean on even when you're tired and your patience is thin.
Consider the standoff over driving—a moment many families face as safety and independence begin to shift. You bring it up, your dad gets defensive, and you're left feeling guilty and powerless. This scene plays out in many homes. By 2050, the number of people over 60 is projected to double to more than 2 billion globally. Families everywhere are trying to figure this out.
The right communication tools can turn these tense moments into opportunities for connection.
One of the kindest and most effective things you can do is learn to listen differently. Active listening isn't just about hearing words; it's about catching the feeling behind them. When your mom complains about her noisy neighbor for the third time, is she really upset about the TV, or is she trying to tell you she's lonely?
Active listening means you:
When you listen this way, you're not just waiting for your turn to talk. You're showing them you're on their side, and that alone can lower the temperature in the room.
This can be a game-changer. Validation is not the same as agreement. You can acknowledge that your parent's feelings are real and legitimate without agreeing with their version of the story.
So when your parent says, "You're always checking up on me! You must think I can't do anything myself," our instinct can be to jump in with, "No, I don't!" But that can sometimes build a wall.
Try validating the feeling first. "I can see how it would be so frustrating to feel like you're being watched. That must be very difficult."
When someone feels truly heard and understood, they often become more open to hearing another perspective. It's a sequence that can really matter: validate first, discuss second.
It can help to have a few phrases ready. These aren't about manipulation; they're about framing your concerns with love so your parent can actually hear you.
Here are a few ways to reframe common conflicts:
Instead of: "You can't drive anymore."
Try: "Dad, I love how independent you are. I've been getting worried about how busy the roads are lately. It would give me so much peace of mind if we could look at some other options for you to get around, just as a backup."
Instead of: "This rug is a hazard. You have to get rid of it."
Try: "Mom, I noticed this rug slips a little bit. I would feel so much better if we could either tape it down or maybe find a pretty new one that stays flat. Your safety is the most important thing to me."
Instead of: "Are you having trouble paying your bills?"
Try: "I was just sorting through my own finances and realized how complicated everything is getting. Would it be helpful if I came over to help you organize the paperwork? Sometimes a second set of eyes makes it easier."
See the shift? These scripts start with "I feel" and focus on teamwork ("we") instead of accusation ("you"). That simple change can make all the difference.
The thought of setting a boundary with a parent can feel strange, or even selfish. But it can be one of the most loving things you can do—for you and for them. Boundaries aren't about building a wall; they're about preventing the burnout and resentment that can quietly erode the relationship you both cherish.
Think of it as creating a sustainable way to care. It's how you protect your own energy so you can continue to show up as the calm, patient, and caring person you want to be.
These moments often signal the need for clearer, more compassionate boundaries that protect both your relationship and your own well-being.
Being there for your parent doesn't mean being on call for every single thing, at all hours of the day. Their anxiety or loneliness is very real, but it doesn't have to become your constant crisis to solve. An important step is learning to tell the difference between a true emergency and a recurring emotional need.
If you're feeling overwhelmed by endless calls, you're not alone. This is a common challenge. The global elderly care market is evolving, growing to meet the needs of an aging population, which shows how many of us are trying to figure this out.
Making this distinction can be the difference between a relationship built on mutual respect and one that's headed for exhaustion.
Saying "no" can feel incredibly hard, especially when you're the go-to person for help. The key is to pair compassion with firmness. You can acknowledge their need while still holding your limit.
Here are a few ways that can work:
Every time you say "no" to something that isn't truly urgent, you're saying "yes" to your own well-being. And that's what allows you to be a better, more present support for them in the long run. If this is a big struggle, our article on setting boundaries with aging parents goes into more detail.
A boundary isn't a wall you build to keep people out. It's a line you draw to protect the space where you and your parent can have a healthy, loving relationship.
The constant ringing of the phone can be one of the most draining parts of this journey. Those calls, often driven by anxiety or loneliness, can shatter your focus at work and interrupt family time. The goal isn't to stop talking; it's to create a structure that works for everyone.
Try setting up a predictable schedule for calls. You could say something like, "Dad, I love our talks. How about we plan to have a good catch-up call every evening around 7 p.m.? That way, I can give you my full attention."
This simple shift accomplishes two things:
This isn't about ignoring them. It's about structuring your communication so that it honors their need for connection and your need for peace. It puts you back in control of your day while still delivering consistent, loving care.
One of the hardest lessons for a caregiver can be admitting you can't do it all yourself. This isn't a sign of failure—it's a sign of strength. Recognizing you need a team is a powerful step toward finding the best possible care for your parent and yourself.
For some families, these conversations eventually connect to broader questions about whether additional support—or a different living environment—might be needed.
Trying to carry the entire weight of caregiving alone can lead to burnout. Building a support network is essential, not just for practical help, but for your own emotional well-being. It gives you people to share the load with, new perspectives, and a shoulder to lean on when it all feels like too much.
The natural first stop for support is usually family. But getting siblings or other relatives on the same page can feel like its own full-time job. The key is to approach these conversations with a clear plan, not just an emotional plea.
Instead of calling a sibling in a moment of frustration, try scheduling a dedicated family meeting. A video call can work well to include everyone, no matter where they live. Your goal is to present the situation calmly and frame it as a team effort.
Here's how you might structure that talk:
Remember, fair doesn't always mean equal. A sibling who lives across the country can't drive your parent to a doctor's appointment, but they can set up grocery deliveries or contribute to a fund for in-home help. The goal is shared responsibility, not identical tasks.
Sometimes, family help isn't enough, or the needs are simply beyond what relatives can handle. This is when bringing in a neutral, trained professional can be a game-changer for everyone.
Seeking outside help isn't admitting defeat. It's a strategic move to preserve family relationships by shifting some of the most difficult burdens to an expert.
These professionals are skilled at navigating the exact challenges you're facing. When a parent resists every suggestion you make, hearing the same advice from an objective third party can sometimes break through the resistance. For more guidance on this common struggle, our article on what to do when aging parents refuse help offers additional strategies.
Here is a simple decision guide that can help you visualize when it might be time to take action, especially when setting boundaries feels impossible.
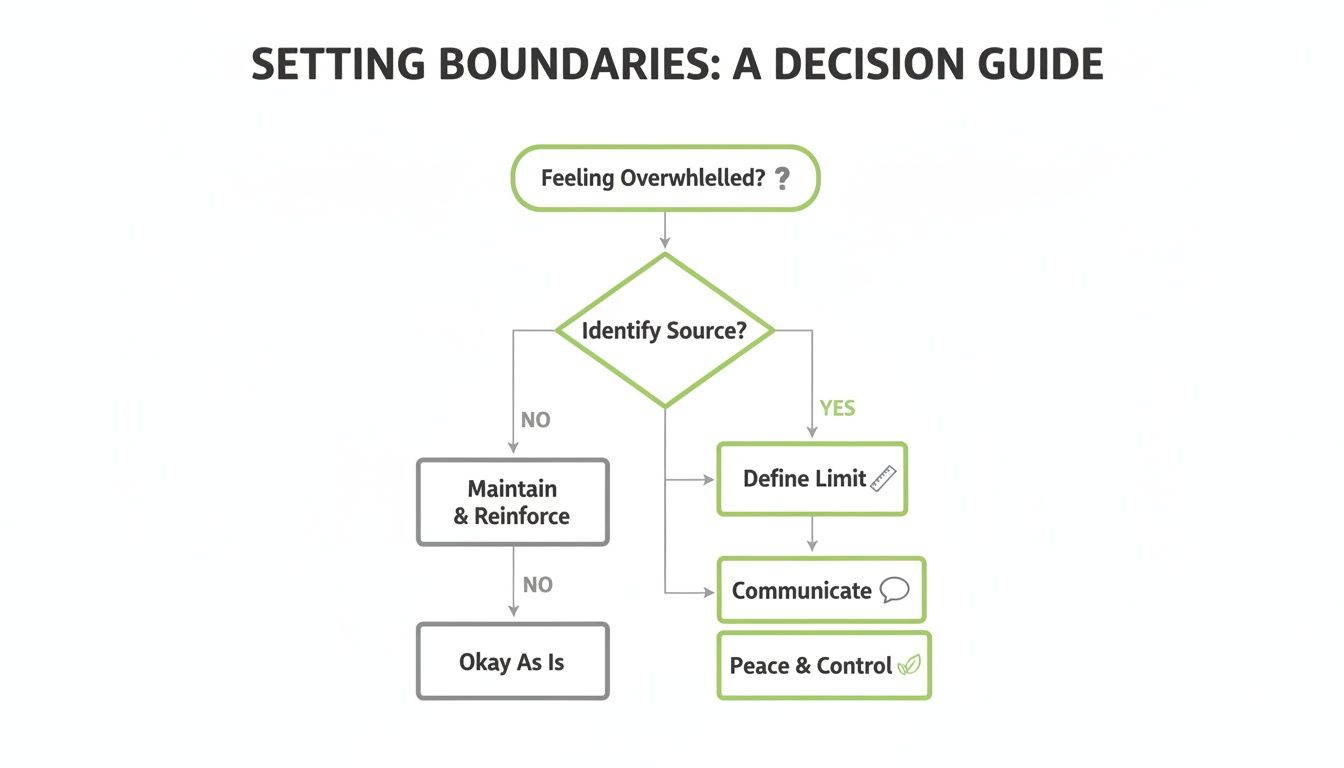
The flowchart shows that recognizing your own feelings of overwhelm is an important first step toward creating a much-needed limit. It all starts there.
So, who are these professionals? While there are many options, here's a look at some of the key people who can step in to guide your family through complex decisions.
This table breaks down some helpful professional roles, what they do, and when you might consider reaching out. They can bring clarity and expertise just when you need it most.
| Type of Support | How They Can Help | When to Consider Reaching Out |
|---|---|---|
| Geriatric Care Manager | Often social workers or nurses specializing in aging. They assess needs, create a care plan, and connect you with local resources. | When you're overwhelmed and don't know where to start, or when your parent's needs become too complex to manage alone. |
| Elder Mediator | A neutral third party who facilitates family conversations about care. They help find common ground and create a plan. | When siblings disagree on the best path forward, or when conversations about care consistently lead to arguments. |
| Elder Law Attorney | Specializes in legal matters affecting older adults, such as wills, trusts, and powers of attorney. | When you need to get legal documents in order, plan for long-term care costs, or protect your parent's assets. |
| Financial Planner | Helps families understand the financial impact of caregiving and create a sustainable plan to pay for long-term care. | When you're worried about how to afford in-home help, assisted living, or other care expenses without depleting savings. |
Having this kind of expert guidance can make a world of difference. It takes the pressure off you to have all the answers and allows you to focus more on your relationship with your parent.

As you navigate this journey with your parent, there's one person whose well-being is incredibly easy to overlook: you. It feels natural to put their needs first. But ignoring your own limits is the surest way to find yourself completely burned out.
This isn't about being selfish; it's about being sustainable. When you're rested and clear-headed, you can meet difficult moments with more patience and compassion. The old saying is true: you can't pour from an empty cup. This is about finding real, practical ways to keep your own cup from running dry.
Caregiver burnout can be a slow burn. It's a creeping exhaustion that can be tough to spot until you're already running on fumes. Catching the early signs gives you a chance to make small changes before you hit a wall.
If you're feeling any of this, know that you're not failing. You're human. These are just your body's signals that you need more support.
Keep an eye out for these common signs:
Just noticing these feelings is a huge first step. The next is giving yourself permission to do something about them, guilt-free.
The idea of "self-care" can feel like just another thing on your to-do list. A spa day or a weekend away might not be realistic.
The key is to think smaller. Much smaller. It's about finding tiny, achievable moments of peace that can actually fit into your life as it is right now. These are often called micro-breaks—quick, intentional pauses to reset your nervous system. They don't take much time, but they add up.
It's not about finding huge blocks of free time. It's about weaving tiny moments of intentional rest into the fabric of your day to keep yourself from unraveling.
Where could you find just five or ten minutes for yourself?
These small acts aren't luxuries. They're essential tools for staying resilient through a challenging time.
Caregiving can bring up some messy emotions. It is completely normal to feel frustrated, resentful, or just plain angry sometimes. You might feel guilty for wishing things were different or for not having an endless supply of patience.
These feelings don't make you a bad son or daughter. They make you a person going through something incredibly difficult. Pushing them down only gives them more power.
One of the kindest things you can do for yourself is find one person you can be totally honest with—a partner, a sibling, a friend who gets it, or a therapist. Having a safe place to say, "This is really hard today," without being judged is a massive relief. There are also caregiver support groups, both online and local, where you can find people who know exactly what you're feeling. You don't have to carry this alone.
Even when you're trying your best, some situations can feel completely stuck. That's okay, and it's certainly normal. Below are a few calm, practical ways to approach some of the most common challenges we hear about from families.
This is, without a doubt, one of the most common and frustrating roadblocks. You see a problem, offer a reasonable solution, and are met with an immediate "No." It feels personal, but it almost never is.
Before you feel discouraged, try to remember what might be underneath that refusal: a deep, human need for control and independence.
So, instead of pushing for a big, sweeping change, shrink your ask. Make it tiny. If you're worried about them falling in the bathroom, don't start by suggesting a walk-in shower. Just start with the mat. "It would really help me worry less if we could put a non-slip mat in the shower. Would you be willing to try that for me?"
Notice the shift? You're framing it around your peace of mind, not their deficit. This little change can sometimes be enough to sidestep their defenses. It might take ten of these tiny conversations to make one small bit of progress, but patience here isn't just a nice idea—it's your most effective tool.
Guilt can be a heavy and painful emotion, especially when it comes from a parent. Comments like, "After all I've done for you..." or "I guess I'll just be all alone then," can make you feel trapped and resentful.
Arguing or defending yourself often backfires. A more powerful response can be quiet, calm consistency.
First, acknowledge the feeling without accepting blame. A simple, "I'm sorry you're feeling lonely today, Mom," is enough. It tells them you hear their sadness.
Then, gently but firmly, restate your boundary. "My intention is never to make you feel that way, and I also have to get the kids to their practice. We'll talk tomorrow morning like we planned." This approach shows that while you care about their feelings, guilt won't change your decision. Over time, it helps them learn that this strategy doesn't work.
Your job isn't to absorb their guilt; it's to respond with calm consistency. Acknowledging their feeling while holding your boundary is the kindest thing you can do for the long-term health of your relationship.
Nothing leads to burnout faster than feeling like you're doing it all alone. The resentment that builds when siblings are absent can fracture relationships when you need them most. The key is to shift the conversation from emotional blame to a structured, practical request.
Try not to call them in a moment of anger. Instead, schedule a time for a family chat—even a 15-minute video call is better than nothing. And go into that call prepared with a specific, manageable list of tasks.
If they still refuse after a calm, direct request, you're facing a difficult truth: you can't force them to change. At that point, your energy is better spent building a support system with friends, other relatives, or professional services—not fighting a battle you can't win. Your well-being has to come first.
At Helping Mom LLC, our goal is to provide the calm, practical, and reassuring guidance you need on this journey. We're here to help you feel less alone and more confident, one step at a time.
Visit Helping Mom